Vitamin D and Its Connection to Diabetes: Insights and Implications
Written on
Understanding Diabetes
Diabetes is a chronic health issue marked by elevated blood sugar levels. A vital player in this condition is vitamin D, which has been shown to influence insulin sensitivity. Insulin, a hormone crucial for managing blood sugar, can be less effective in those with lower vitamin D levels, potentially leading to insulin resistance—a key feature of type 2 diabetes.
The Two Types of Diabetes
In type 1 diabetes, the pancreas fails to produce insulin. This condition is closely associated with vitamin D levels. Specifically, vitamin D activates receptors on the surface of beta cells in the pancreas. These beta cells are responsible for insulin secretion, which is essential for transferring glucose from the bloodstream to cells that require energy. Supplementation with vitamin D can enhance insulin secretion. Research indicates that islets from individuals with vitamin D deficiencies exhibit reduced insulin secretion when stimulated by glucose.
Furthermore, vitamin D has protective effects on beta cells against apoptosis, which is the programmed cell death that occurs due to cytokine signaling. This is particularly relevant in autoimmune conditions that arise from vitamin D deficiency. A lack of vitamin D means that beta cells are not adequately stimulated to produce insulin, leading to dangerously high blood glucose levels, as the body cannot metabolize glucose without sufficient insulin.
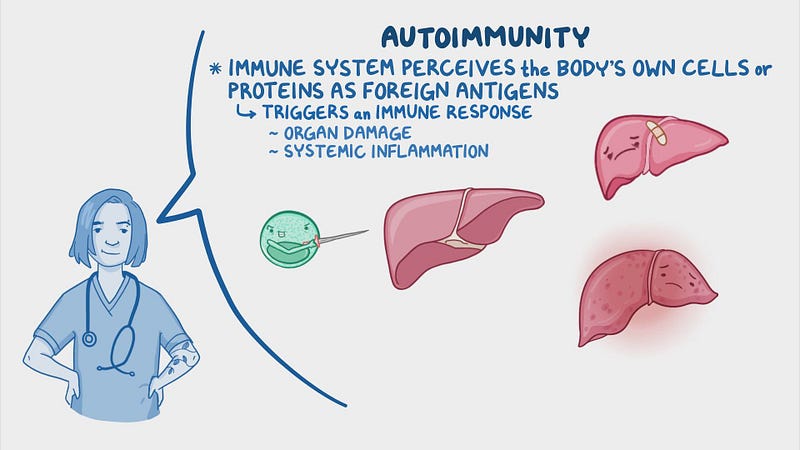
Defining Autoimmunity
The immune system can mistakenly attack insulin-producing beta cells in the pancreas, resulting in autoimmune responses. Therefore, understanding what beta cells are becomes crucial in this context.
Diabetes Type 1: A Summary
In type 1 diabetes, the absence of insulin due to beta cell destruction is the primary issue.
Diabetes Type 2: An Overview
Conversely, in type 2 diabetes, the pancreas still produces insulin but does so in insufficient amounts over time. This type is often characterized by insulin resistance, where the body's cells fail to respond effectively to insulin, leading to elevated blood sugar levels. This condition is more frequently diagnosed in adults, typically after age 40, but is increasingly being seen in children and adolescents due to rising obesity rates and sedentary lifestyles.
Conclusion and Recommendations
In conclusion, both type 1 and type 2 diabetes involve challenges with insulin regulation and blood sugar control, but they differ in their causes, onset age, and management strategies. Type 1 diabetes is an autoimmune disorder with a rapid onset that necessitates lifelong insulin treatment. In contrast, type 2 diabetes is closely linked to lifestyle choices and insulin resistance, often managed through lifestyle modifications and medication; however, insulin therapy may become necessary as the condition progresses.