Herd Immunity: A Renewed Hope Amidst Challenges
Written on
Understanding the Current Landscape
As mask mandates ease across the United States, a sense of relief and optimism fills the air. The long-awaited conclusion of the pandemic appears closer than ever. But what does this really signify?
Throughout much of the pandemic, the concept of herd immunity — the point at which enough individuals have been vaccinated or infected with SARS-CoV-2 to stop its spread — represented hope for overcoming the crisis. We debated the percentage needed for vaccination — whether it was 70%, 80%, or 85% — with a clear aim in sight: true victory over the virus.
However, the vaccination campaign encountered significant obstacles in American society: vaccine skepticism, political debates, and widespread conspiracy theories. Suddenly, the idea of achieving herd immunity felt out of reach. An article in The New York Times proclaimed, “Reaching ‘Herd Immunity’ Is Unlikely in the U.S., Experts Now Believe.” This piece summarizes valid concerns from public health professionals, indicating that while we may not eradicate COVID-19, it can become manageable, akin to living with the flu. This shift in perspective reflects the new guidance from the CDC: while we may not eliminate COVID-19, the effectiveness of vaccines allows us to return to normalcy.
Yet, I refuse to accept this resignation. I firmly believe that we can achieve a genuine victory over SARS-CoV-2 rather than settling for a mere truce. However, this will require effort and determination, which is why I am concerned that the prevailing narrative suggests it's impossible. My intention here is to present several reasons why I believe herd immunity remains attainable.
Vaccine Hesitancy: A Deeper Look
Firstly, vaccine hesitancy may not be as severe as often assumed. Recent surveys indicate that hesitancy is declining, though around 30% of adults still report they won’t get vaccinated. The encouraging news is that many of these individuals are still persuadable. A small fraction, perhaps 10%, may be staunchly opposed, but the majority could be convinced. The Johnson & Johnson vaccine, which requires only one shot, can effectively convert some of the unvaccinated into the vaccinated. Thus, improving accessibility — making vaccines readily available at locations like Walmart and local pharmacies — is crucial.
Mathematics of Herd Immunity
The second reason for optimism in achieving herd immunity is mathematical. The threshold for herd immunity is not arbitrary; it relates to the basic reproduction number of the virus, which indicates how many people an infected individual can pass the virus to under normal circumstances.
If an infected person infects, on average, two others, herd immunity could be reached with just 50% of the population protected. Current estimates suggest the R0 of SARS-CoV-2 is approximately 2.5, which implies a herd immunity threshold of around 70%. This figure includes children, who represent about 25% of the U.S. population, making the goal challenging yet feasible, particularly as vaccination efforts expand to younger age groups.
Moreover, the effective reproduction number, which reflects the current transmission dynamics, can also be influenced by non-vaccine measures like mask-wearing and social distancing. In fact, modeling indicates that prior to widespread vaccination, the effective reproduction number was already reduced to about 1.2.
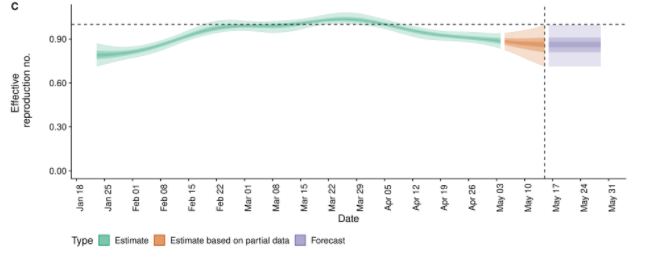
In essence, even if we can't achieve herd immunity solely through vaccination, we can reach it through a combination of vaccination and continued preventive measures. Therefore, if you haven’t been vaccinated yet, please maintain social distancing and mask-wearing to keep the effective reproduction number low.
Natural Immunity: An Alternative Path
The third point is often overlooked: individuals can still gain immunity without vaccination. While vaccination is the preferred method due to the risks associated with COVID-19, if we can’t vaccinate enough individuals, natural infections will occur — primarily among the unvaccinated — which will elevate the overall immunity in the community. This approach isn’t ideal but does contribute to herd immunity.
Addressing the Variant Challenge
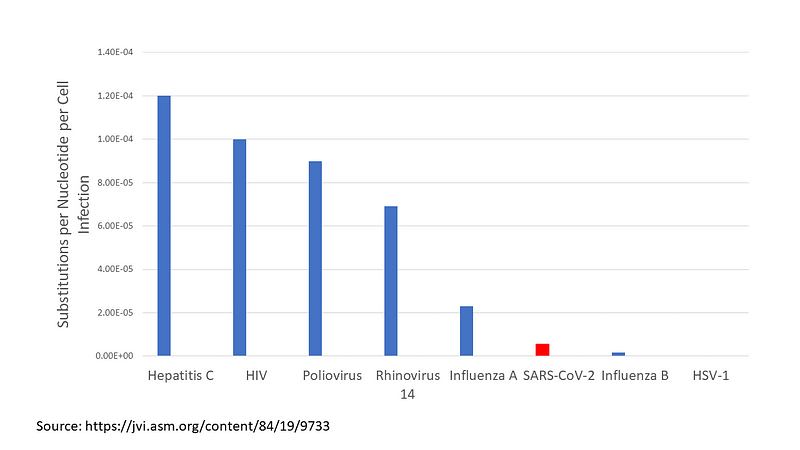
Fourthly, the emergence of variants may not be as detrimental as some fear. While SARS-CoV-2 is known to mutate, it does so at a slower rate compared to many other viruses. The high volume of infections provides numerous opportunities for genetic changes, but as case numbers decrease, the rate of variant emergence is likely to decline as well.
The rapid development of vaccines also provides hope. Though it took a year to begin widespread vaccinations, Moderna had a prototype ready even before the first case was reported in the U.S. RNA vaccine technology may allow us to adapt quickly to any emerging variants, minimizing potential impacts if we can keep case numbers low.
Global Perspective on Vaccination
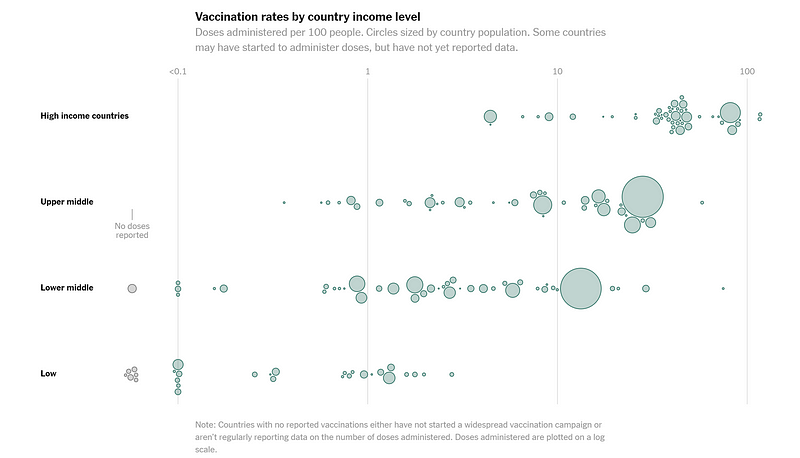
Lastly, we must consider the global vaccination landscape. While achieving 80% vaccination in the U.S. is a goal, we also face disparities worldwide. Currently, North America has administered 54 doses for every 100 people, compared to just 1.7 doses per 100 people in Africa. This inequality underscores the importance of global vaccination efforts; COVID-19 does not adhere to borders.
Local herd immunity can act as a firewall against further transmission, suggesting that while we focus on our own vaccination efforts, we can simultaneously aid other nations in their vaccination campaigns.
In summary, we find ourselves at a pivotal moment. Public sentiment appears to be shifting towards accepting COVID-19 as an ongoing presence rather than aiming for its eradication. However, we still have the opportunity to commit to the hard work of vaccinating both our nation and the world, ultimately overcoming this global challenge. It's not impossible — it's simply a difficult journey.
Music video highlighting the importance of vaccination in the fight against COVID-19.
An insightful message addressing concerns of those hesitant to receive the COVID vaccine.